Treating Chronic Wounds with Smart Bandages Cheaply, Easily, and Effectively
Over time, your body naturally heals burns, scrapes, cuts, and other wounds. But when someone has diabetes, the body’s natural healing process becomes impaired; thus, some wounds take a long time to heal, and their persistence makes them susceptible to infection, which can worsen. Doctors call them chronic wounds. Chronic wounds are more prevalent in individuals with diabetes, as the condition impairs the body’s healing process.
Chronic wounds cause substantial emotional and physical distress and put a considerable financial burden on the healthcare system, which, on average, costs about $25 billion per year.
A novel smart bandage
Researchers at Caltech developed a new type of smart bandage to treat chronic wounds easily, effectively, and cheaply. They developed the smart bandage at the lab of the assistant professor of medical engineering, Wei Gao. He is also a Ronald and JoAnne Willens scholar and a Heritage Medical Research Institute Investigator.
According to Asst. Prof. Gao, there is a huge demand for technology that can help the recovery of people with different types of chronic wounds, particularly burns, non-healing surgical wounds, and diabetic ulcers that last for some time.
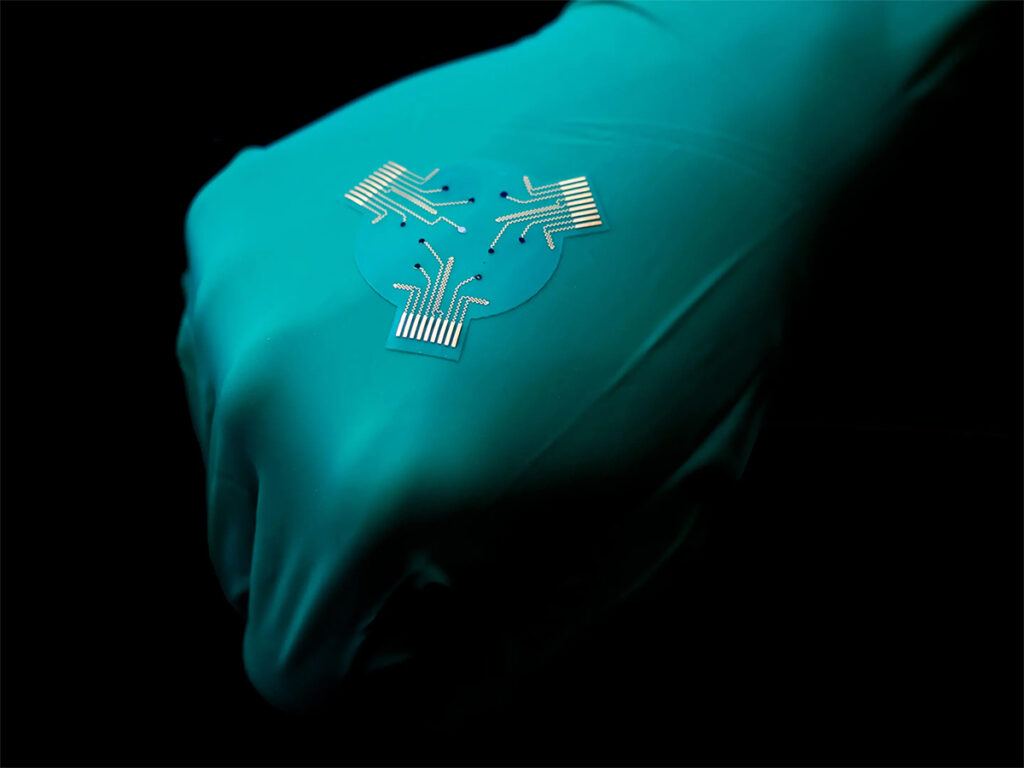
A typical bandage comprises layers of absorbent materials; however, the smart bandage, which sticks to the skin, uses a stretchy and flexible polymer with medication and electronics embedded in it. The device has a disposable patch and a reusable flexible printed circuit board. The disposable part contains drug-loaded hydrogels, electrodes, and biosensors.
The electronics has a sensor that monitors glucose, lactate, or uric acid molecules and conditions such as temperature in the wound or pH level that may indicate a bacterial infection or inflammation.
Bandage response
The smart bandage responds in different ways. It can wirelessly transmit collected data from the wound to a nearby computer, smartphone, or tablet. The patient or a medical practitioner can review the data. The smart bandage can likewise deliver a controlled and targeted dose of the required medication or antibiotic stored within the bandage. The delivery of the medicine is direct to the wound site. Finally, the smart bandage can give the wound a low-level electrical field to stimulate tissue growth and facilitate healing.
Lab results
Using lab animal models in laboratory settings, the smart bandages exhibited their ability to give real-time updates about the conditions of the wounds and the metabolic states of the lab animals. Simultaneously, the smart bandage promoted speed healing of chronically infected wounds.
The researchers also found that the lab mice with smart bandages receiving electrical stimulation and drug release had higher wound closure rates. Moreover, they exhibited less scarring compared to lab animals that did not have bandages covering their wounds.
Mr. Gao said they got promising results, and their future research collaborating with USC’s Keck School of Medicine will concentrate on improving bandage technology and human testing because human patients’ therapeutic needs could differ from the needs of laboratory animals. In addition, they are looking at increasing the stability of the device and testing it on larger chronic wounds in human patients.
The future of smart bandages
The research team expects the production cost of smart bandages to be about tens of dollars for the device’s reusable electronics part. The disposable patch would cost a few dollars. Currently, the smart bandage lasts for up to two weeks.
Since the team needs to work further on the device and conduct studies on pigs and humans, the team leader hopes clinics can use the smart bandages in five to ten years, which is good news for individuals with chronic wounds.
